C3.2.3 VACCINATION AND IMMUNE MEMORY
📌Definition Table
| Term | Definition |
|---|---|
| Vaccine | A preparation of antigens that stimulates adaptive immunity without causing disease. |
| Immunisation | The process of inducing immunity via vaccination. |
| Herd immunity | Protection of unvaccinated individuals when a critical proportion of a population is immune. |
| Booster dose | A repeated vaccination that enhances memory and prolongs immunity. |
| Attenuated vaccine | Vaccine using weakened but live pathogens. |
| Subunit vaccine | Vaccine containing only parts of a pathogen (proteins, polysaccharides) that trigger immunity. |
📌Introduction
Vaccination harnesses adaptive immunity by exposing individuals to harmless forms of antigens, priming memory B and T cells for future encounters with the pathogen. This creates a rapid, strong secondary immune response upon real infection. Vaccination not only protects individuals but also communities through herd immunity. Modern biotechnology has expanded vaccine types, including mRNA and recombinant vaccines. However, challenges remain in vaccine distribution, hesitancy, and evolving pathogens
📌 How Vaccines Work
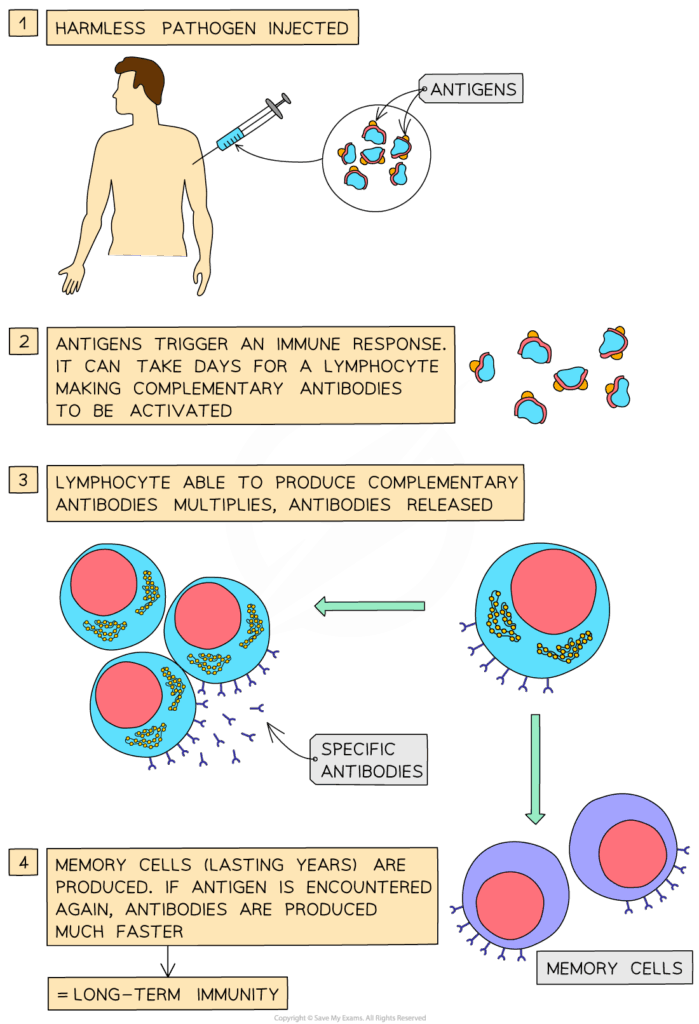
- Vaccines introduce antigens without causing full disease.
- Stimulate clonal selection of B and T cells → formation of memory cells.
- On re-exposure, immune memory produces rapid, high-level responses.
- Can use whole pathogens (killed/attenuated) or components (subunits, toxoids).
- New technologies: mRNA vaccines instruct cells to produce pathogen proteins, triggering immunity.
🧠 Examiner Tip: Always explain that vaccines do not provide immediate protection — they prepare immune memory for future encounters.
📌 Types of Vaccines
- Live attenuated: strong, long-lasting immunity; risk in immunocompromised patients (e.g., measles, polio Sabin).
- Inactivated: killed pathogens; safer but often weaker response (e.g., influenza).
- Subunit: only antigens, very safe but need boosters (e.g., HPV).
- Toxoid: inactivated toxins (e.g., tetanus, diphtheria).
- mRNA and vector-based: cutting-edge, highly effective, adaptable to new pathogens (e.g., COVID-19 vaccines).
🧬 IA Tips & Guidance: Investigations can model vaccine impact using simulations of herd immunity, showing how increasing vaccination rates reduce disease spread.
📌 Immune Memory and Boosters
- Vaccines create memory B and T cells for long-term protection.
- Booster shots re-stimulate memory cells, raising antibody levels.
- Some vaccines provide lifelong immunity (measles), others need regular boosters (tetanus, flu).
- Immune memory explains why childhood vaccinations are scheduled in series.
- Variability in pathogen mutation rates affects duration of immunity.
🌐 EE Focus: An EE could compare immune memory durability across vaccine types, or analyse how mutation rates (e.g., influenza vs measles) affect vaccination strategies.
📌 Herd Immunity and Public Health
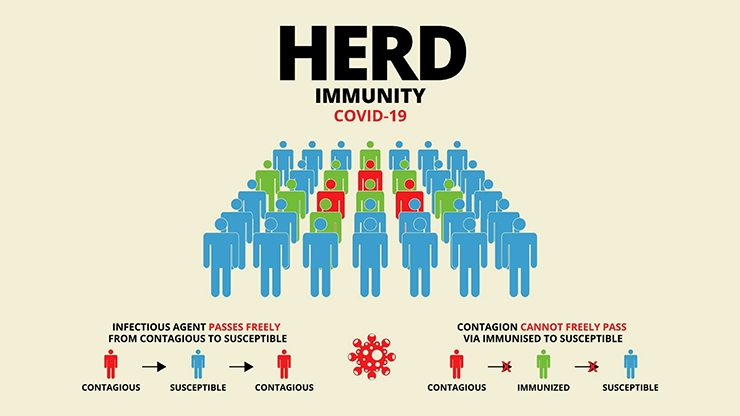
- Herd immunity occurs when enough people are immune, limiting pathogen spread.
- Protects vulnerable groups (infants, elderly, immunocompromised).
- Requires high vaccination coverage; threshold depends on pathogen transmissibility.
- Public trust, education, and access determine success of herd immunity.
- Loss of herd immunity (due to hesitancy) can trigger disease resurgence.
❤️ CAS Link: Students could run awareness projects on the importance of vaccines in their community, addressing myths and highlighting global equity issues.
🌍 Real-World Connection: COVID-19 demonstrated the power of rapid vaccine development, but also the challenges of equitable access and misinformation. Vaccination campaigns remain central to eradicating diseases like polio and measles.
📌 Challenges and Ethical Issues
- Pathogen mutation (antigenic drift/shift in influenza) requires frequent updates.
- Vaccine hesitancy threatens public health.
- Ethical dilemmas: mandatory vaccination vs individual freedom.
- Global inequality: low-income countries struggle with access and infrastructure.
- Future vaccines may target chronic diseases (e.g., cancer, HIV).
🔍 TOK Perspective: Vaccines raise TOK issues about knowledge, trust, and uncertainty. Scientific evidence strongly supports vaccination, but social perspectives (beliefs, values) influence acceptance. TOK question: How does trust in science shape public health decisions?